Third-party medical billing is a process where healthcare providers outsource their billing tasks to external agencies. These agencies specialize in handling the complex and time-consuming aspects of medical billing, such as claim submissions, follow-ups, and payment collections. This service is particularly beneficial for medical practices of all sizes that want to focus on patient care rather than administrative tasks.
Utilizing third-party medical billing becomes essential when in-house billing becomes overwhelming, error-prone, or inefficient, leading to delayed reimbursements and financial instability for the healthcare provider.
What is Third-Party Medical Billing?
Third-party medical billing, also known as 3rd party billing, involves outsourcing the billing process to a specialized agency that handles claim submissions and follow-ups on behalf of healthcare providers. These agencies are experts in navigating the complexities of medical billing codes, insurance regulations, and reimbursement procedures.
By partnering with a third-party billing service, healthcare practices can ensure that their claims are accurately processed and submitted in a timely manner, leading to improved reimbursement rates and reduced administrative burdens.
This allows medical professionals to focus on providing quality patient care rather than being bogged down by billing issues.
Why Businesses Use Third-Party Medical Billing?
Businesses opt for third-party medical billing services to streamline their administrative processes and enhance overall efficiency. Handling medical billing in-house can be time-consuming and prone to errors, which can delay reimbursements and negatively impact a practice’s cash flow.
Third-party billing agencies employ experienced professionals who stay updated on the latest healthcare regulations and coding changes, ensuring accurate and timely claim submissions. Additionally, outsourcing billing tasks allows healthcare providers to reduce overhead costs associated with hiring and training in-house billing staff.
How Does Third-Party Medical Billing Work?
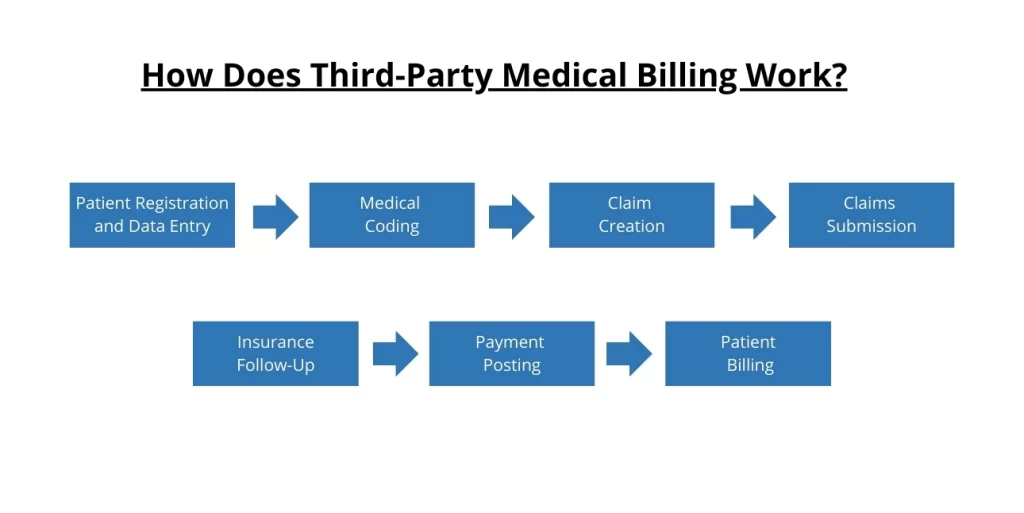
Third-party medical billing involves a systematic process where healthcare providers and billing companies collaborate to manage billing tasks efficiently. The healthcare providers focus on patient care and documentation, while the third-party billing companies handle the intricate billing procedures.
Patient Registration and Data Entry: The healthcare provider collects patient information and medical details, which are then entered into the system.
Medical Coding: The provider’s documentation is translated into standardized billing codes (CPT, ICD-10) by either the provider or the billing company.
Claim Creation: The third-party billing company uses these codes to generate claims that are compliant with insurance requirements.
Claims Submission: The billing company submits the claims electronically to the appropriate insurance carriers.
Insurance Follow-Up: The billing company tracks the submitted claims, handles any rejections or denials, and resubmits if necessary.
Payment Posting: Once payments are received, the billing company posts them to the patient accounts and reconciles any discrepancies.
Patient Billing: Any remaining balance is billed to the patient, and the billing company manages collections if needed.
Benefits of Third Part Medical Billing?
Outsourcing medical billing to third-party agencies offers numerous advantages that can significantly enhance the efficiency and financial health of healthcare practices. By leveraging specialized expertise, these services ensure accurate claim submissions and faster reimbursements, which can improve cash flow and reduce administrative burdens.
Here are some of the key benefits of medical billing outsourcing:
Improved Accuracy
One of the primary medical billing outsourcing advantages is the increased accuracy in claim submissions. Third-party billing companies employ experts who are well-versed in the latest coding standards and insurance regulations. This reduces the likelihood of errors, which can lead to claim denials and delays.
Cost Savings
Outsourcing medical billing can lead to significant cost savings. By eliminating the need for in-house billing staff, healthcare practices can reduce overhead expenses such as salaries, benefits, and training costs. This allows practices to allocate resources more effectively.
Enhanced Focus on Patient Care
Medical billing outsourcing allows healthcare providers to focus more on patient care rather than administrative tasks. With billing responsibilities handled by experts, providers can dedicate more time to improving patient outcomes and overall service quality.
Faster Reimbursements
Third-party billing companies streamline the claim submission process, leading to quicker reimbursements from insurance companies. Their expertise in follow-ups and dealing with denials ensures that claims are processed efficiently, reducing the time it takes to receive payments.
Access to Advanced Technology
Billing companies often use state-of-the-art technology and software to manage claims. This not only enhances the accuracy and speed of the billing process but also provides healthcare providers with access to advanced reporting and analytics, helping them make informed financial decisions.
Regulatory Compliance
Staying compliant with ever-changing healthcare regulations can be challenging. Third-party billing companies stay updated on the latest laws and ensure that all billing practices adhere to current standards, reducing the risk of compliance-related issues and penalties.
Reduced Administrative Burden
Outsourcing billing tasks significantly reduces the administrative burden on healthcare staff. This allows office personnel to concentrate on other essential tasks, such as patient scheduling and care coordination, improving the overall efficiency of the practice.
Improved Cash Flow
By ensuring timely and accurate claim submissions, third-party billing services can help improve cash flow. Faster reimbursements and reduced claim denials mean that practices receive payments more promptly, enhancing financial stability and growth potential.
Key Players in Third-Party Medical Billing
The third-party medical billing process involves several key players, each playing a crucial role in ensuring smooth and efficient billing operations. Understanding the roles and interactions of these players can help clarify the overall billing process.
1. Healthcare Providers
Healthcare providers are the primary source of medical services and documentation. They collect patient information, diagnose conditions, and provide treatments. Providers ‘ accurate documentation is essential for proper coding and billing.
They collaborate with third-party billing companies by sharing necessary patient and service details, ensuring that the billing process begins accurately.
2. Third-Party Billing Companies
Third-party billing companies specialize in managing the billing process for healthcare providers. They are responsible for translating medical services into standardized billing codes, creating and submitting claims to insurance companies, and following up on claim statuses.
Their expertise in medical billing ensures accuracy, compliance, and efficiency, leading to timely reimbursements and reduced administrative burdens for healthcare providers.
3. Insurance Companies
Insurance companies play a critical role in the reimbursement process. They review the submitted claims to verify coverage, determine the amount payable, and either approve or deny the claims based on their policies and the accuracy of the submissions.
Insurance companies work closely with third-party billing companies to resolve any issues with claims and ensure that reimbursements are processed as quickly as possible.
4. Patients
Patients are the recipients of medical services and are ultimately responsible for any out-of-pocket expenses not covered by their insurance. They provide necessary information to healthcare providers and may need to communicate with both providers and billing companies regarding their bills.
Patients also benefit from third-party billing services, as these companies can offer clear and accurate billing statements, making it easier for patients to understand their financial responsibilities and make payments promptly.
Things to Consider When Outsourcing to a 3rd Party Billing Provider
Outsourcing medical billing to a third-party provider can greatly enhance efficiency and profitability for healthcare practices. However, choosing the right provider is crucial to ensure you receive the best possible service. Here are some key factors to consider when selecting a third-party billing provider:
Experience and Expertise: Ensure the provider has extensive experience and expertise in medical billing, particularly in your specialty. Look for a company with a proven track record of handling similar practices.
Compliance and Security: Verify that the provider adheres to all healthcare regulations, including HIPAA, to protect patient information. Their security measures should be robust to prevent data breaches.
Technology and Integration: Assess the technology the provider uses and ensure it integrates seamlessly with your existing systems. Advanced, user-friendly software can streamline the billing process and improve efficiency.
Transparency and Reporting: The provider should offer comprehensive and transparent reporting on all billing activities. This includes regular updates on claim statuses, reimbursements, and any issues that arise.
Service Scope and Support: Understand the full scope of services the provider offers and ensure they align with your needs. Check their support availability to ensure you can get help when needed.
Financial Terms and Costs: Compare the financial terms and costs of different providers. Look for a provider that offers competitive rates without compromising on service quality.
References and Reviews: Seek references from other healthcare providers who have used the billing service. Reviews and testimonials can provide insights into the provider’s reliability and performance.
Flexibility and Scalability: The provider should be flexible and able to scale their services as their practice grows or changes. This ensures they can meet your evolving needs.
Communication and Customer Service: Effective communication is crucial. Ensure the provider offers excellent customer service and maintains clear, responsive communication channels.
Contractual Terms: Carefully review the contractual terms, including the length of the contract, termination clauses, and any other legal stipulations. Ensure they are fair and protect your interests.
The Bottom Line
Third-party medical billing serves as a pivotal solution for healthcare providers looking to streamline their administrative processes and improve financial efficiency. By outsourcing billing tasks to specialized agencies, providers can focus more on delivering quality patient care while ensuring accurate and timely reimbursement.
This approach not only reduces administrative burdens but also enhances overall practice management, making third-party medical billing a valuable asset in today’s healthcare landscape.






