Interoperability in healthcare is revolutionizing the way medical information is shared and utilized across the industry. This crucial concept refers to the ability of different healthcare systems and software applications to communicate, exchange, and interpret shared data effectively.
In medical billing, interoperability plays a pivotal role in streamlining processes, ensuring accurate data exchange, and minimizing billing errors, thereby contributing to a more efficient and patient-centered healthcare system.
What is Interoperability?
Interoperability refers to the capability of diverse healthcare information systems, devices, and applications to access, exchange, integrate, and cooperatively use data in a coordinated manner. This functionality ensures that the information shared across different healthcare settings is clear, accurate, and actionable, regardless of the technology or software in use.
In healthcare, interoperability is essential for creating a connected ecosystem where patient data can flow seamlessly between electronic health records (EHRs), laboratory systems, imaging devices, and billing systems.
This connectivity not only enhances clinical decision-making but also improves operational efficiency and patient outcomes by enabling timely and accurate information exchange across the healthcare continuum.
Interoperability Components
Interoperability in healthcare comprises several key components that work together to ensure effective data exchange and integration. These components facilitate the seamless flow of information across various systems and platforms, enabling healthcare providers to deliver coordinated and high-quality care. Understanding these components is crucial for leveraging interoperability to its fullest potential.
Technical Interoperability: Involves the technical requirements for systems to communicate, such as data formats, protocols, and standards that allow different IT systems to exchange and use information.
Semantic Interoperability: Ensures that the meaning of exchanged data is understandable and consistently interpreted across different systems, achieved through common data models, terminologies, and coding systems.
Organizational Interoperability: Refers to the ability of different organizations to effectively communicate and collaborate, supported by shared processes, policies, and agreements.
Process Interoperability: Focuses on the workflow and business processes that support the coordination of care, including data-sharing agreements and the integration of health IT systems into clinical workflows.
Foundational Interoperability: The basic level that allows one information system to receive data from another but may not include the capability to interpret the data.
What is the Principle of Interoperability?
The principle of interoperability is founded on the idea that healthcare systems should be capable of working together seamlessly to improve patient care and operational efficiency. This principle emphasizes the importance of standardization, collaboration, and communication among disparate health IT systems.
By adhering to agreed-upon standards and protocols, different healthcare entities can ensure that their systems can exchange and use information in a meaningful way. This involves not only the technical aspects of data exchange but also the semantic understanding and organizational alignment required for coherent and effective communication.
The ultimate goal of interoperability is to create a cohesive and integrated healthcare ecosystem where information flows freely and accurately, enhancing clinical decision-making, reducing redundancies, and improving overall patient outcomes.
Challenges of Interoperability in Healthcare
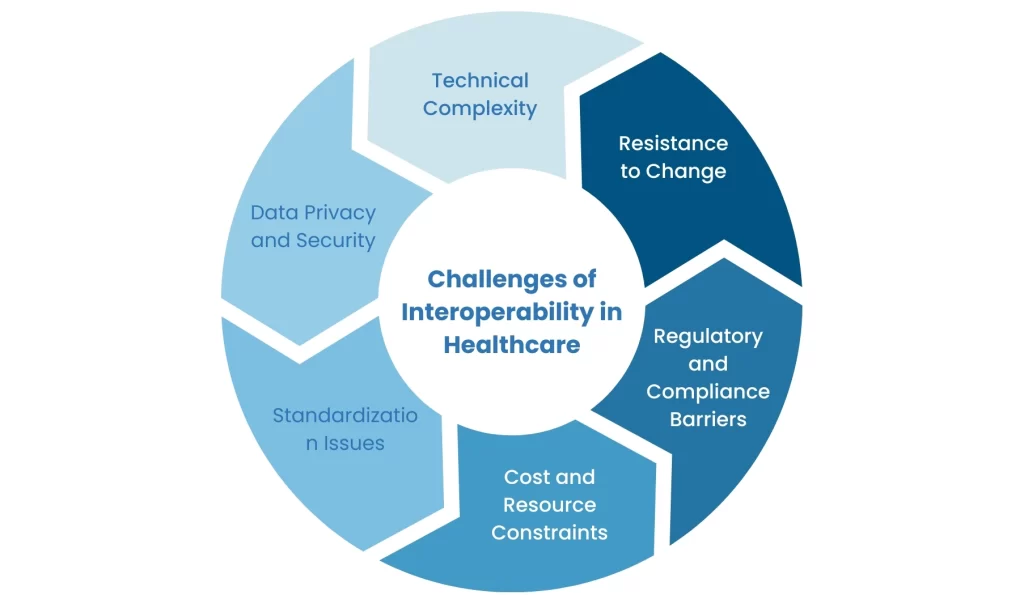
While the benefits of interoperability in healthcare are substantial, several challenges must be addressed to achieve seamless data integration and communication. These challenges often arise from technical, organizational, and regulatory barriers that complicate the implementation and maintenance of interoperable systems.
Technical Complexity: Integrating diverse systems with varying architectures, data formats, and protocols can be highly complex and resource-intensive.
Data Privacy and Security: Ensuring the confidentiality, integrity, and availability of sensitive patient information while facilitating data exchange is a significant concern.
Standardization Issues: The lack of universally accepted standards and terminologies can lead to inconsistencies and misinterpretations of shared data.
Cost and Resource Constraints: Implementing and maintaining interoperable systems requires significant financial investment and technical expertise, which may be challenging for smaller healthcare providers.
Regulatory and Compliance Barriers: Navigating the diverse and often stringent regulatory requirements across different regions and institutions can hinder the smooth exchange of healthcare information.
Resistance to Change: Healthcare organizations may face resistance from staff and stakeholders who are accustomed to existing workflows and systems, making the transition to interoperable solutions challenging.
What is Interoperability Important in Healthcare?
The importance of interoperability in healthcare cannot be overstated. It serves as the backbone for efficient and effective data exchange across various healthcare systems and platforms.
By enabling seamless communication and integration, interoperability ensures that healthcare providers have access to accurate and up-to-date patient information, which is crucial for delivering high-quality care.
The benefits of interoperability in healthcare extend beyond clinical outcomes, impacting operational efficiency, patient safety, and overall healthcare costs.
Enhancing Clinical Decision-Making
One of the primary benefits of interoperability in healthcare is the enhancement of clinical decision-making. When healthcare providers have access to comprehensive patient data, including medical history, test results, and treatment plans, they can make more informed decisions. This holistic view of the patient’s health status reduces the likelihood of errors and ensures that care is tailored to the individual’s needs.
Improving Patient Safety
The importance of interoperability in healthcare is also evident in its role in improving patient safety. By facilitating real-time data exchange between different healthcare entities, interoperability helps in identifying potential issues such as drug interactions, allergies, and duplicate tests. This timely access to critical information can prevent medical errors and adverse events, ultimately protecting patient health.
Streamlining Operations
Another significant benefit of interoperability in healthcare is the streamlining of operations. Interoperable systems reduce administrative burdens by automating data entry and sharing processes.
This not only saves time but also reduces the risk of human error. Efficient data management and communication can lead to cost savings and better resource allocation within healthcare organizations.
Enhancing Patient Experience
Interoperability also plays a crucial role in enhancing the patient experience. When healthcare providers have seamless access to patient records, it reduces the need for patients to repeatedly provide the same information.
This continuity of care fosters better patient-provider relationships and improves overall satisfaction. Additionally, patients can access their own health information more easily, empowering them to take an active role in their healthcare journey.
Facilitating Public Health and Research
The importance of interoperability in healthcare extends to public health and research as well. Interoperable systems enable the aggregation and analysis of large datasets, providing valuable insights into health trends and outcomes.
This data can inform public health strategies, support evidence-based practice, and drive medical research, ultimately leading to advancements in healthcare and better population health management.
The Bottom Line
Interoperability enables seamless communication and data exchange across various healthcare systems, ensuring that providers have access to accurate and timely information. This not only enhances clinical decision-making and patient safety but also streamlines operations and improves the overall patient experience.
As healthcare continues to evolve, achieving full interoperability will be crucial in delivering high-quality, coordinated, and efficient care. Embracing interoperability is not just about technology—it’s about building a connected and collaborative healthcare ecosystem that benefits providers, patients, and the broader community.






