Feeling lost when it comes to mental health billing? You are not alone. Many therapists and mental health professionals find dealing with insurance claims, reimbursement rates, and coding to be confusing and stressful. But getting mental health billing right is important for making sure you get paid fairly for your work and that your patients aren’t burdened with unexpected costs.
In this guide, we’ll explain the basics of mental health billing, how reimbursement works, and give you tips to make the process easier. Whether you’re new to billing or just need a refresher, this guide will help you get on track and keep your practice running smoothly.
How Is Mental Health Billing Different From Medical Billing?
Mental health billing differs from general medical billing in several key ways. While both involve managing insurance claims and reimbursement, mental health billing requires specific coding and documentation tailored to the nuances of mental health care.
For example, mental health services often use different coding systems, such as ICD-10 codes for mental health disorders, which are distinct from those used for physical ailments.
Additionally, the billing process for mental health can involve unique considerations like session notes that detail the therapeutic approach and progress, which aren’t typically required for other medical fields.
Why Mental Health Billing is Complicated?
Mental health billing is complicated due to several factors that make it more challenging than standard medical billing. Firstly, the coding for mental health services is complex and must accurately reflect the complexity of mental health conditions and treatments.
Therapists and counselors often need to use specific codes for each diagnosis and treatment, which can vary widely and change frequently. Additionally, the reimbursement rates for mental health services can be lower or more variable compared to other medical services, creating financial uncertainty.
The requirement for detailed and precise documentation to justify the need for therapy or counseling further adds to the complexity. Combined with insurance policies that may have unique rules or limitations for mental health coverage, navigating the billing process can be a daunting task for many professionals in the field.
Types of Mental Health Services
Mental health services encompass a broad range of treatments and interventions designed to address various psychological, emotional, and behavioral issues. These services can be tailored to individual needs and may include everything from routine therapy sessions to specialized interventions. Here’s a breakdown of the key types of mental health services:
- Individual Therapy: One-on-one sessions between a therapist and a client focusing on personal issues and goals.
- Group Therapy: Sessions with multiple participants guided by a therapist, offering support and shared experiences.
- Family Therapy: Involves family members working together with a therapist to address dynamics and improve relationships.
- Couples Therapy: Focuses on improving communication and resolving conflicts between partners.
- Crisis Intervention: Immediate support and stabilization during acute mental health emergencies.
- Psychiatric Evaluations: Comprehensive assessments by a psychiatrist to diagnose mental health conditions and determine appropriate treatment.
- Medication Management: Monitoring and adjusting medication for patients with mental health conditions.
- Substance Abuse Counseling: Specialized therapy aimed at helping individuals overcome addiction and related issues.
Each of these services has its own billing requirements and documentation needs, making it essential for mental health professionals to understand and accurately manage the billing process for each type of care provided.
Diagnosis Coding for Mental Health Billing
Diagnosis coding is a critical component of mental health billing, as it ensures that the services provided are accurately represented and reimbursed. For mental health services, such as psychotherapy, specific codes are used to describe various conditions and guide treatment. These codes are essential for insurance claims and must be precise to reflect the patient’s diagnosis correctly.
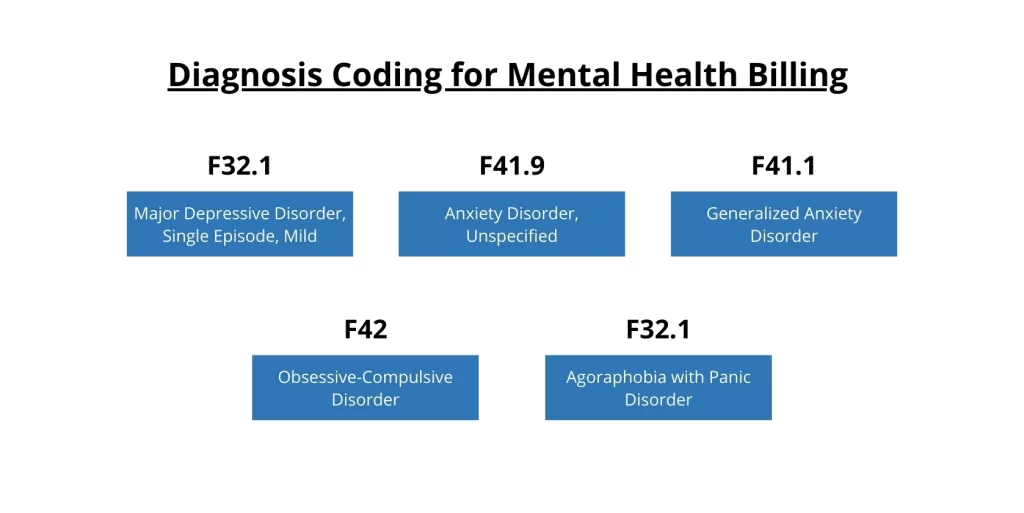
Here are some common diagnosis codes used in mental health billing:
F32.1 Major Depressive Disorder, Single Episode, Mild: Used for patients experiencing a mild single episode of major depression.
F41.9 Anxiety Disorder, Unspecified: A general code for anxiety disorders when the exact type is not specified.
F41.1 Generalized Anxiety Disorder: For patients with persistent and excessive worry about various aspects of life.
F42 Obsessive-Compulsive Disorder: Applied when a patient exhibits persistent, unwanted thoughts and repetitive behaviors.
F32.1 Agoraphobia with Panic Disorder: Used for individuals who experience severe anxiety about being in situations where escape might be difficult or help might not be available.
Commonly Used Mental Health CPT Codes
Understanding commonly used CPT (Current Procedural Terminology) codes is essential for accurate mental health billing. These codes help specify the type of service provided and ensure that billing and reimbursement are processed correctly. Here are some frequently used CPT codes in mental health services:
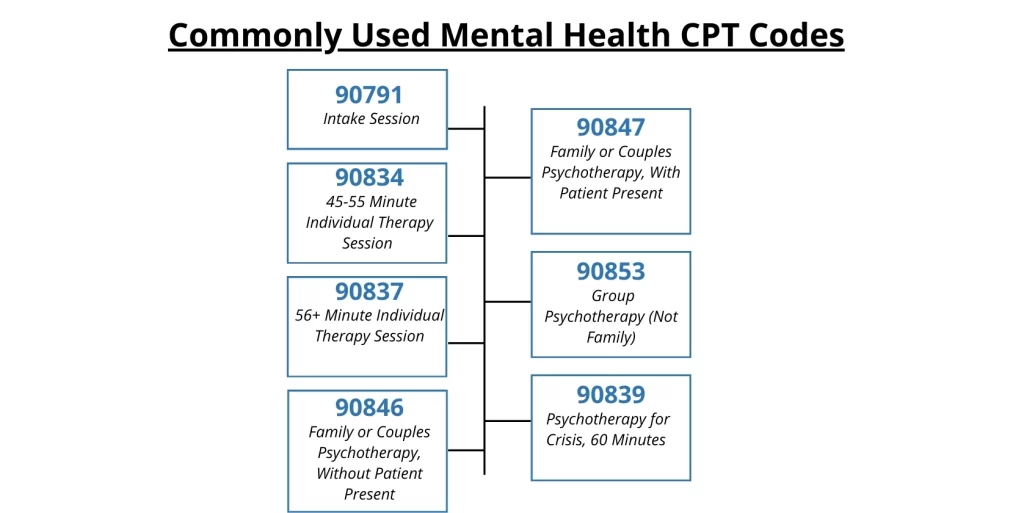
- 90791: Intake Session — This code is used exclusively for the first appointment with a new patient, during which a comprehensive assessment is conducted.
- 90834: 45-55 Minute Individual Therapy Session — This code is for a standard therapy session lasting between 45 and 55 minutes.
- 90837: 56+ Minute Individual Therapy Session — Used for longer therapy sessions that last over 56 minutes.
Other Common Behavioral Health CPT Codes:
- 90846: Family or Couples Psychotherapy, Without Patient Present — This code is used when providing therapy to family members or couples without the patient being present.
- 90847: Family or Couples Psychotherapy, With Patient Present — This code is for family or couples therapy where the patient is present during the session.
- 90853: Group Psychotherapy (Not Family) — Used for group therapy sessions that do not include family members.
- 90839: Psychotherapy for Crisis, 60 Minutes — Applied for crisis intervention sessions lasting between 30 and 74 minutes.
How To Submit Claims in Mental Health Billing
Submitting claims in mental health billing involves several key steps to ensure that your claims are processed efficiently and accurately. Start by gathering all necessary documentation, including detailed session notes, diagnosis codes, and CPT codes for the services rendered.
Complete the claim form, usually the CMS-1500 form for outpatient services, ensuring all fields are filled out correctly with the relevant information. Double-check that all codes and documentation align with the patient’s diagnosis and treatment plan to avoid rejections or denials.
Once the claim is prepared, submit it to the insurance company through their preferred method, whether electronically or by mail. Monitoring the status of your claims is crucial; follow up on any denials or requests for additional information promptly to resolve issues and ensure timely reimbursement.
Proper submission and follow-up are essential for maintaining a smooth billing process and ensuring that your practice receives the compensation it deserves.
Who Can Bill for Mental Health Services?
Billing for mental health services can be done by a range of qualified professionals, each with their own set of credentials and expertise. Here’s a look at who can bill for mental health services:
Licensed Therapists: This group includes professionals such as psychologists, Licensed Clinical Social Workers (LCSWs), and Licensed Professional Counselors (LPCs). These individuals are trained to provide therapy and counseling, and they are typically credentialed to submit claims for their services.
Psychiatrists: These medical doctors specialize in mental health and are qualified to manage medications as well as provide therapy. Their advanced training allows them to address complex mental health conditions and bill for both medication management and therapeutic services.
Incident-to Billing: Under certain circumstances, non-physician providers can bill for mental health services if they work under the supervision of a physician. This includes cases where a licensed therapist performs services that are overseen by a physician, ensuring compliance with billing regulations.
Credentialing and Insurance Panels: Providers must be credentialed and approved by insurance panels to bill for services. This process ensures that they meet the required standards and are recognized by insurance companies for reimbursement.
Scope of Practice: Billing practices must align with the scope of practice as defined by state regulations. Each state has specific rules about what services different types of mental health professionals can provide and bill for.
Specialized Training: Professionals with specialized training in certain therapies or for specific patient groups can also bill for these services. This includes advanced training in particular therapeutic techniques or working with specialized populations.
Closing Note
Mental health billing doesn’t have to be overwhelming. By understanding the basics of diagnosis codes, CPT codes, and the billing process, you can make sure that your practice gets paid correctly and on time. Knowing who can bill and how to handle claims properly will help you avoid mistakes and ensure smooth operations.
With a clear grasp of these key aspects, you can focus more on helping your patients and less on billing issues, keeping your practice both efficient and financially secure.