Medical billing and coding is an essential behind-the-scenes procedure in the complex field of healthcare that guarantees the efficient operation of medical facilities and the smooth provision of patient care. Simply put, medical billing and coding is the systematic translation of healthcare services into universal alphanumeric codes for billing and insurance claims.
Medical billing and coding serve as the backbone of the healthcare revenue cycle, ensuring that healthcare providers receive rightful compensation for their services while facilitating efficient communication between providers, payers, and patients.
What is Medical Billing and Coding?
Medical billing and coding are two distinct yet interrelated processes essential for the financial health of healthcare providers and the accessibility of care for patients.
Medical coding involves translating medical diagnoses, procedures, and services into universal alphanumeric codes. These codes are derived from various coding systems, such as the International Classification of Diseases (ICD) and the Current Procedural Terminology (CPT).
On the other hand, medical billing is the process of submitting these coded claims to insurance companies or patients for reimbursement. It involves verifying patient information, checking insurance eligibility, and ensuring compliance with regulatory requirements.
| Aspect | Medical Coding | Medical Billing |
| Definition | Translating medical diagnoses and procedures into universal alphanumeric codes. | Submitting coded claims to insurance companies orpatients for reimbursement. |
| Key Components | ICD, CPT, HCPCS codes | Patient information verification, insurance eligibility check, regulatory compliance |
| Example | Assigning ICD-10 code for a diagnosis of diabetes mellitus. | Submitting a claim with CPT codes for a routine office visit to an insurance company for reimbursement. |
Why is Medical Billing and Coding Important?
In the complex ecosystem of healthcare, medical billing and coding play pivotal roles in ensuring the financial stability of healthcare providers and facilitating smooth interactions between providers, payers, and patients.
Importance of Medical Billing
Medical billing serves as the financial backbone of healthcare facilities, ensuring that healthcare providers receive timely and accurate reimbursement for the services they render.
Without efficient medical billing processes, healthcare providers would struggle to maintain financial viability, leading to potential disruptions in patient care and facility operations.
Timely reimbursement enables healthcare providers to invest in resources, technology, and staff training, ultimately enhancing the quality of patient care.
Why is Medical Coding Important?
Medical coding is the language of healthcare, translating complex medical diagnoses, procedures, and services into universally recognized alphanumeric codes. These codes are crucial for accurately documenting patient encounters and medical necessity, which in turn impacts reimbursement rates and claims processing.
Without accurate coding, healthcare providers risk revenue loss due to claim denials, undercoding, or coding errors. Additionally, precise medical coding ensures compliance with regulatory requirements and facilitates data analysis for research, quality improvement, and healthcare policy formulation.
Types of Medical Coding
Medical coding encompasses various code sets, each serving specific purposes within the healthcare industry. The primary types of medical coding include:
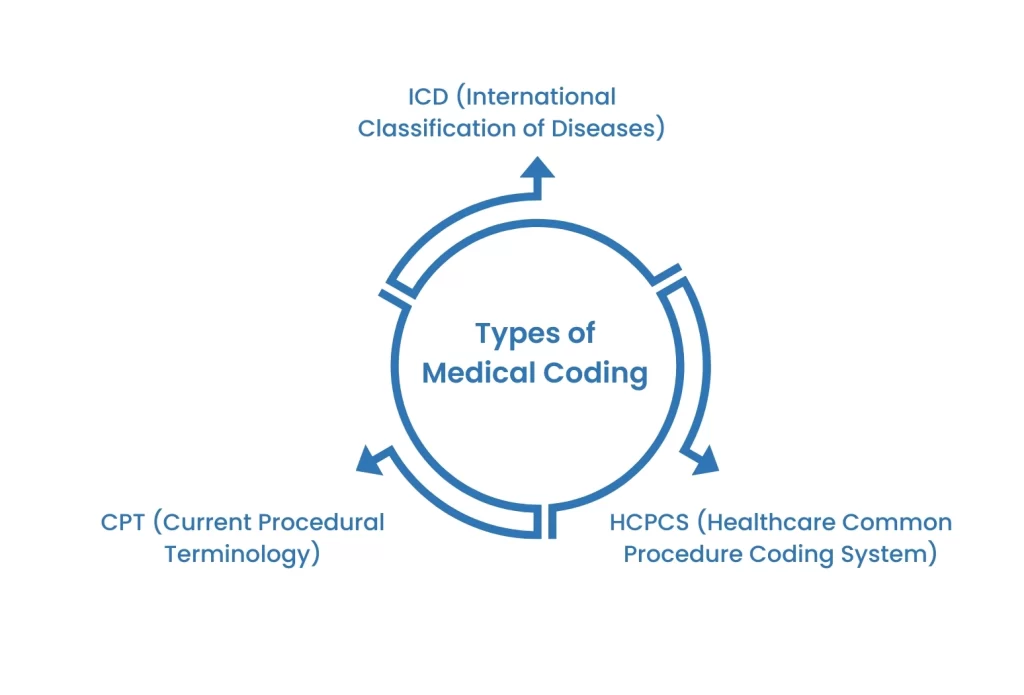
1. ICD (International Classification of Diseases): ICD codes capture diagnoses and provide a standardized method for classifying diseases and health-related conditions. The current version, ICD-10, offers a comprehensive framework for coding diagnoses and morbidity data, enabling accurate documentation and statistical analysis.
2. CPT (Current Procedural Terminology): CPT codes represent medical procedures and services provided by healthcare professionals. Developed by the American Medical Association (AMA), CPT codes facilitate accurate billing and reimbursement for a wide range of medical services, from office visits to surgical procedures.
3. HCPCS (Healthcare Common Procedure Coding System): HCPCS codes are used primarily for Medicare and Medicaid billing purposes. This coding system includes two levels of codes: Level I (CPT codes) and Level II (national alphanumeric codes), covering services, supplies, and equipment not included in the CPT code set.
What is the Role of a Medical Billing Specialist?
A medical billing specialist, also known as a medical biller, plays a multifaceted role in the healthcare revenue cycle, encompassing tasks ranging from coding and billing to claims processing and revenue management. Here’s a breakdown of their key responsibilities:
Coding and Documentation: One of the primary responsibilities of a medical billing specialist is to translate medical diagnoses, procedures, and services into standardized alphanumeric codes using coding systems such as ICD-10 and CPT. They meticulously review medical records and documentation to ensure accuracy and compliance with regulatory requirements, thereby facilitating proper reimbursement for healthcare services.
Claims Submission and Management: Medical billing specialists are responsible for preparing and submitting insurance claims to various payers, including private insurance companies, Medicare, and Medicaid. They navigate the complexities of insurance policies, verify patient eligibility, and follow up on claim statuses to ensure timely reimbursement. Additionally, they handle claim denials and appeals, advocating for healthcare providers to maximize reimbursement and minimize revenue loss.
Patient Billing and Account Management: Beyond insurance claims, medical billing specialists also oversee patient billing and account management processes. They generate patient statements, calculate co-pays, deductibles, and coinsurance amounts, and assist patients with billing inquiries and payment arrangements.
By maintaining accurate and transparent billing practices, they contribute to positive patient experiences and foster trust in healthcare providers.
Revenue Cycle Optimization: Medical billing specialists play a crucial role in optimizing the healthcare revenue cycle by identifying inefficiencies, streamlining processes, and implementing best practices to maximize revenue and minimize financial risks.
They collaborate with other healthcare professionals, such as physicians, nurses, and administrative staff, to ensure alignment between clinical operations and financial objectives.
Compliance and Regulatory Adherence: In an ever-evolving regulatory landscape, medical billing specialists must stay abreast of changes in healthcare laws, regulations, and coding guidelines.
They ensure compliance with federal and state regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) and the Affordable Care Act (ACA), to safeguard patient privacy and maintain ethical billing practices.
Steps in the Medical Billing Process
The medical billing process involves a series of crucial steps to ensure accurate reimbursement for healthcare services rendered. From patient registration to claims submission, each stage plays a vital role in the revenue cycle of healthcare providers. Here’s an overview of the key steps involved:
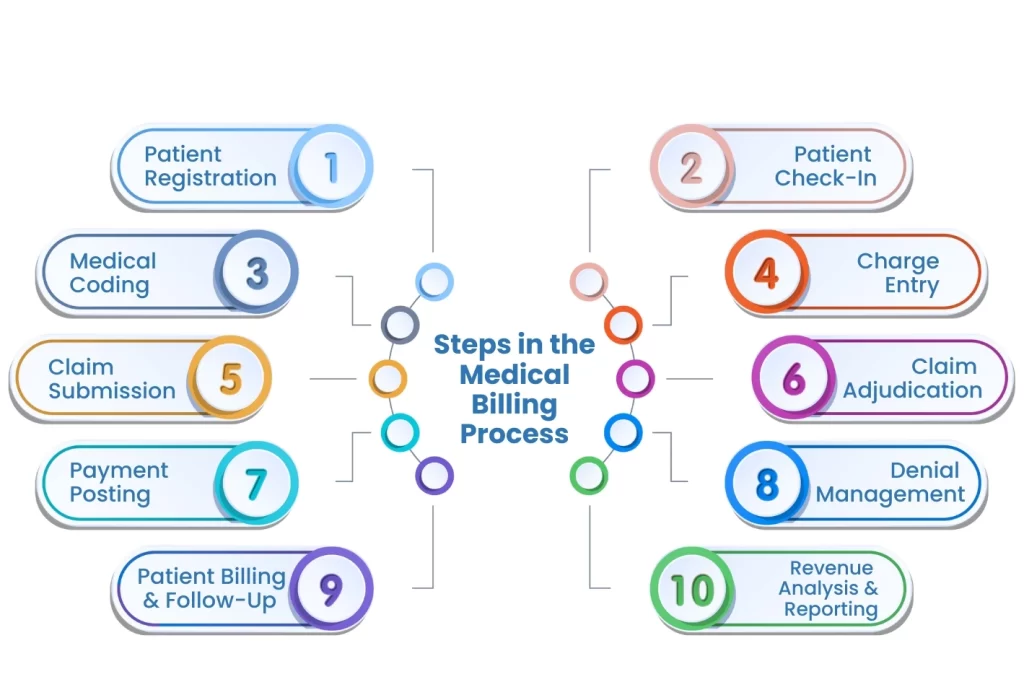
Patient Registration: The process begins with capturing patient demographic and insurance information accurately. This step is essential for verifying insurance coverage and determining patient responsibility for payment.
Patient Check-In: Upon arrival, patients provide updated information and sign consent forms. Front desk staff collect co-payments, deductibles, and outstanding balances, if applicable.
Medical Coding: Healthcare services, diagnoses, and procedures documented during patient encounters are translated into standardized alphanumeric codes using coding systems such as ICD-10 and CPT.
Charge Entry: Once coded, charges for medical services are entered into the billing system, specifying the type and quantity of services provided.
Claim Submission: Completed claims are submitted electronically or via mail to insurance companies or government payers for reimbursement. Claims include patient information, diagnosis codes, procedure codes, and provider details.
Claim Adjudication: Insurance companies review claims for accuracy, medical necessity, and coverage eligibility. Adjudicated claims result in either payment, denial, or request for additional information.
Payment Posting: Upon receipt of payment from insurance companies or patients, payments are recorded and applied to patient accounts accordingly. Any remaining balances are billed to patients or secondary insurance.
Denial Management: Denied claims are reviewed, corrected, and resubmitted with necessary documentation or appeals. Denial reasons are analyzed to identify and address root causes to minimize future claim rejections.
Patient Billing and Follow-Up: Patient statements are generated for outstanding balances, including co-pays, deductibles, and coinsurance amounts. Follow-up communication is conducted to address billing inquiries and facilitate payment arrangements.
Revenue Analysis and Reporting: Regular monitoring and analysis of billing data, reimbursement trends, and key performance indicators (KPIs) inform strategic decision-making and revenue cycle optimization efforts.
How Does Outsourcing Medical Billing and Coding Services Benefit Physicians?
Outsourcing medical billing and coding services can offer numerous benefits to physicians and medical practices, allowing them to focus on delivering high-quality patient care while streamlining administrative tasks and maximizing revenue potential.
By partnering with experienced billing and coding professionals, physicians can alleviate the burden of managing complex billing processes in-house, leading to improved operational efficiency and financial performance.
Outsourcing ensures access to specialized expertise and up-to-date knowledge of evolving healthcare regulations and coding guidelines, minimizing errors and claim denials.
Moreover, outsourcing allows physicians to reduce staffing costs, overhead expenses, and technology investments associated with maintaining an in-house billing department.
With dedicated support from outsourcing partners, physicians can optimize revenue cycle management, enhance practice profitability, and dedicate more time to clinical activities and patient engagement.
The Bottom Line
The importance of medical billing and coding cannot be overstated in the realm of healthcare administration. These processes serve as the linchpin of the revenue cycle, ensuring accurate documentation, timely reimbursement, and regulatory compliance for healthcare providers.
By understanding the critical role of medical billing and coding, healthcare organizations can optimize financial performance, enhance operational efficiency, and ultimately, deliver better patient care.